If you’re experiencing similar fears, take a deep breath. Here’s something many families don’t realize: memory problems don’t always mean Alzheimer’s disease.
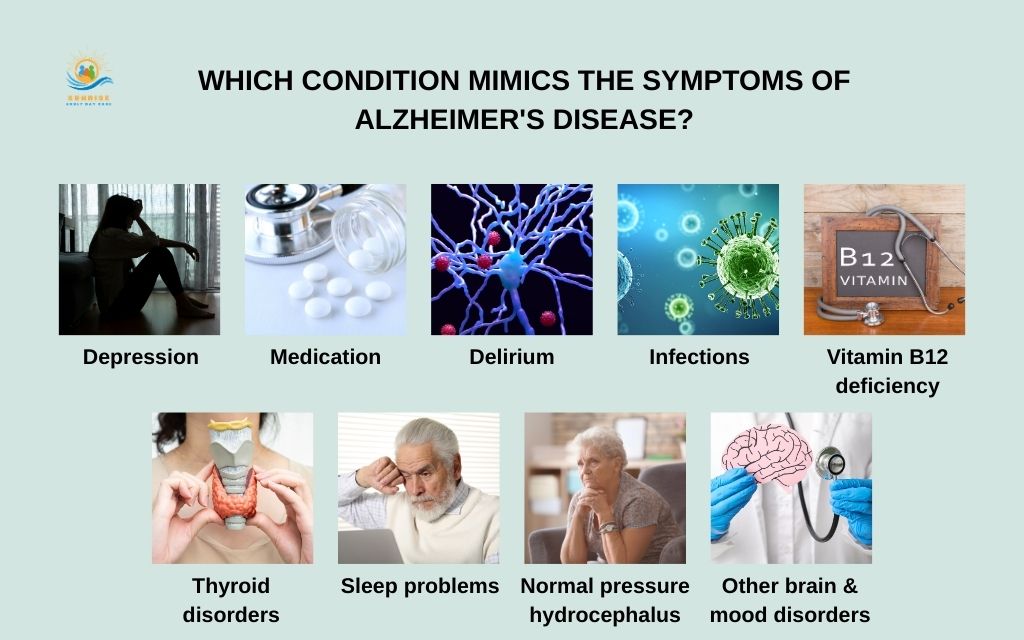
In fact, several other conditions can cause dementia-like symptoms, and importantly, many of these are treatable or even completely reversible. So, which condition mimics the symptoms of Alzheimer’s disease?
This guide will walk you through 9 conditions that can mimic Alzheimer’s symptoms, explain how they differ from true dementia, and most importantly, show you what steps to take next. Understanding that cognitive changes have multiple possible causes – some of which can be addressed – offers something invaluable: hope.
This article is for informational purposes only and does not constitute medical advice. Always consult qualified healthcare professionals regarding cognitive symptoms and medical concerns.
Why so many conditions can mimic dementia
To understand what conditions can mimic symptoms of dementia, we first need to recognize how the brain functions and why it’s vulnerable to so many different disruptions.
Your brain is an incredibly complex organ that depends on:
- Adequate oxygen and blood flow to deliver nutrients
- Proper chemical balance (hormones, neurotransmitters, electrolytes)
- Essential nutrients like B vitamins and glucose
- Clear signaling pathways between brain cells
- Sufficient rest through quality sleep
When any of these requirements aren’t met, the brain responds with symptoms that look remarkably similar to dementia:
- Memory loss and forgetfulness
- Confusion and disorientation
- Trouble concentrating or following conversations
- Personality or mood changes
- Slowed thinking
Here’s a crucial distinction: “dementia” is a syndrome, not a single disease. Think of it as an umbrella term describing a group of symptoms that affect cognitive function severely enough to interfere with daily life.
Alzheimer’s disease is the most common cause of dementia, accounting for 60-80% of cases, but it’s far from the only one.
Which condition mimics the symptoms of Alzheimer’s disease?
Condition #1: Depression (“Pseudodementia”)
What disorder is most often misdiagnosed as dementia? The answer might surprise you: depression in older adults.
Depression doesn’t always look like sadness in seniors. Instead, it can present as what clinicians call “pseudodementia” – cognitive symptoms caused by depression that can look remarkably similar to true dementia:
- Memory problems (particularly difficulty recalling recent information)
- Slowed thinking and processing
- Poor concentration and inability to focus
- Withdrawal from previously enjoyed activities
- Lack of motivation or initiative

Condition #2: Medication side effects & drug interactions
One of the most overlooked yet common things that mimic dementia sits right in your medicine cabinet. Older adults often take multiple medications – a practice called polypharmacy – and certain drugs can significantly impair cognitive function:
Common culprits include:
- Anticholinergic medications (some allergy medicines, overactive bladder drugs, sleep aids like diphenhydramine)
- Benzodiazepines (anxiety medications such as lorazepam or diazepam)
- Sleep medications (particularly “Z-drugs” like zolpidem)
- Opioid pain medications
- Some blood pressure medications
- Antihistamines (including over-the-counter products)
These medications can cause:
- Confusion and disorientation
- Memory issues and “brain fog”
- Drowsiness and falls
- Difficulty concentrating
Condition #3: Delirium
Delirium represents one of the most urgent conditions on this list of diseases that cause confusion – it’s a medical emergency that requires immediate attention.
Delirium is characterized by a sudden change in thinking, attention, and awareness that develops over hours to days. Unlike the gradual progression of Alzheimer’s, delirium hits fast and hard.
Common triggers include:
- Infections (urinary tract infections, pneumonia)
- Surgery or hospitalization (particularly after anesthesia)
- New medications or medication changes
- Dehydration or electrolyte imbalances
- Severe pain
- Alcohol withdrawal
Condition #4: Infections (UTIs, pneumonia, COVID-19)
Infections represent another critical category of diseases that cause confusion in older adults and they often present very differently in seniors than in younger people.
In older adults, infections frequently present with cognitive changes as the primary or only symptom. This is because the aging immune system responds differently, often without mounting a fever.
Urinary tract infections (UTIs)
UTIs are notorious for causing delirium and confusion in seniors. Symptoms may include:
- Sudden confusion or worsening memory
- Agitation or behavioral changes
- Increased falls
- Decreased appetite
Importantly, older adults with UTIs may not have the classic symptoms of burning during urination or urgency.
Pneumonia and respiratory infections
Lung infections can cause:
- Mental status changes
- Confusion and disorientation
- Lethargy or unusual sleepiness
- Sometimes without obvious coughing or breathing difficulties initially
COVID-19 and other systemic infections
Recent research has shown that COVID-19 can cause significant cognitive symptoms, sometimes referred to as “brain fog,” both during acute illness and as part of long COVID. Other systemic infections, including sepsis (a life-threatening whole-body response to infection), can also present primarily with altered mental status.

Condition #5: Vitamin B12 deficiency & other nutritional problems
Vitamin B12 deficiency represents one of the more common yet easily treatable conditions that mimic dementia. The good news? It’s detectable through simple blood tests and often reversible with treatment.
Vitamin B12 plays a crucial role in:
- Maintaining the protective coating around nerves (myelin sheath)
- Supporting red blood cell production (which carries oxygen to the brain)
- Enabling proper nerve signaling
When B12 levels drop too low, the nervous system suffers, causing symptoms that can easily be mistaken for dementia:
- Memory loss and forgetfulness
- Confusion and difficulty concentrating
- Mood changes (depression or irritability)
- Numbness or tingling in hands and feet
- Difficulty walking or balance problems
- Fatigue and weakness
Older adults face higher risk for B12 deficiency because:
- Stomach acid production decreases with age
- Certain medications (like metformin for diabetes or proton pump inhibitors for heartburn) interfere with B12 absorption
- Dietary factors (vegetarian/vegan diets, poor nutrition)
- Autoimmune conditions (pernicious anemia)
Condition #6: Thyroid disorders & other hormonal imbalances
Thyroid problems represent another category of diseases similar to dementia that are both common in older adults and highly treatable once identified.
The thyroid gland produces hormones that regulate metabolism throughout the body—including brain metabolism. When thyroid function goes awry, cognitive symptoms often follow.
Hypothyroidism
When the thyroid produces too little hormone, it can cause:
- Memory problems and forgetfulness
- Slowed thinking (“mental sluggishness”)
- Difficulty concentrating
- Depression and mood changes
- Fatigue and lethargy
- Weight gain
- Cold intolerance
These symptoms develop gradually and can easily be attributed to “normal aging” when, in fact, they signal a treatable condition.
Hyperthyroidism
Less commonly, an overactive thyroid can cause:
- Anxiety and nervousness
- Difficulty concentrating
- Memory problems
- Irritability
- Racing thoughts
- Weight loss
- Heat intolerance
Other hormonal culprits
While thyroid disorders are most common, other hormonal imbalances can also affect cognition:
- Adrenal disorders (Cushing’s disease or Addison’s disease)
- Parathyroid problems (affecting calcium levels)
- Changes in sex hormones (though less commonly causing dementia-like symptoms)

Condition #7: Sleep problems
Chronic sleep problems represent a frequently overlooked cause of what mimics dementia – yet they’re surprisingly common and treatable.
During sleep, your brain:
- Consolidates memories from the day
- Clears toxic waste products through the glymphatic system
- Repairs and restores neural connections
- Processes emotions and experiences
When sleep is consistently disrupted, cognitive function suffers dramatically.
Obstructive sleep apnea (OSA)
Sleep apnea involves repeated pauses in breathing during sleep, depriving the brain of oxygen. It’s particularly common in older adults and can cause:
- Poor concentration and “brain fog”
- Short-term memory problems
- Daytime confusion or grogginess
- Irritability and mood changes
- Morning headaches
- Excessive daytime sleepiness
The cognitive effects result from both oxygen deprivation and fragmented sleep that prevents reaching restorative deep sleep stages.
Chronic insomnia and sleep deprivation
Even without apnea, chronic insomnia or severe sleep deprivation can produce dementia-like symptoms:
- Forgetfulness
- Difficulty concentrating
- Slowed reaction time
- Poor decision-making
Condition #8: Normal pressure hydrocephalus (NPH)
Normal Pressure Hydrocephalus might sound complicated, but it represents an important – and treatable – cause of dementia like illness that every family should know about.
NPH occurs when cerebrospinal fluid (the protective fluid surrounding the brain and spinal cord) builds up in the brain’s fluid-filled spaces (ventricles), causing them to enlarge and press on brain tissue.
Despite the “normal pressure” name (referring to normal opening pressure on spinal tap), this condition causes real neurological problems.
NPH is famous for three characteristic symptoms that often appear together – sometimes remembered by the mnemonic “wet, wacky, and wobbly“:
Walking and balance problems (wobbly)
- Shuffling gait
- Difficulty initiating steps
- Feeling “stuck” when starting to walk
- Frequent falls
Urinary incontinence (wet)
- Urgency (sudden, strong need to urinate)
- Frequency
- Loss of bladder control
Cognitive decline (wacky)
- Slowed thinking
- Memory problems
- Difficulty planning or organizing
- Apathy or mood changes
Condition #9: Other brain & mood disorders
The final category encompasses several disorders similar to dementia that deserve attention because they either represent different diseases requiring different approaches, or they’re treatable conditions affecting cognition.
Mild cognitive impairment (MCI)
MCI occupies a middle ground between normal age-related memory changes and dementia:
Characteristics:
- Noticeable memory or thinking problems (beyond normal aging)
- Problems confirmed by testing, but not severe enough to significantly interfere with daily activities
- Daily function mostly intact
Anxiety disorders and chronic stress
Anxiety doesn’t just affect mood – it can significantly impair cognition:
- “Brain fog” and difficulty concentrating
- Forgetfulness (especially when anxious)
- Trouble making decisions
- Difficulty following conversations
Chronic stress floods the brain with cortisol, which can impair memory formation and retrieval. These symptoms often improve with anxiety treatment through therapy, medication, stress management techniques, and lifestyle changes.
Other neurodegenerative diseases
Several other brain diseases can present with symptoms similar to Alzheimer’s but differ in important ways:
Vascular dementia
- Caused by reduced blood flow to the brain (often from strokes or small vessel disease)
- Symptoms may appear suddenly or stepwise rather than gradually
- Often involves executive function problems (planning, organizing) more prominently than memory initially
- Prevention focuses on controlling cardiovascular risk factors (blood pressure, diabetes, cholesterol)
Lewy body dementia
- Caused by abnormal protein deposits (Lewy bodies) in the brain
- Characterized by visual hallucinations, movement problems (similar to Parkinson’s), fluctuating cognition, and sleep disturbances (acting out dreams)
- Requires different medications than Alzheimer’s—some drugs used for Alzheimer’s or behavioral problems can worsen Lewy body dementia
Frontotemporal dementia (FTD)
- Typically affects younger individuals (50s-60s) more than Alzheimer’s
- Personality and behavior changes often appear before memory problems
- May involve language difficulties
Parkinson’s disease dementia
- Develops in some people with Parkinson’s disease
- Movement symptoms typically precede cognitive symptoms by years

Common “look-alike” symptoms to watch for
Understanding 3 symptoms or conditions that could be mistaken for dementia helps you know when to seek evaluation. These overlapping symptoms appear in many conditions—not just Alzheimer’s:
Memory loss and forgetfulness
- Forgetting recent conversations or events
- Asking the same questions repeatedly
- Misplacing items frequently
- Forgetting appointments
Confusion about time or place
- Losing track of dates or seasons
- Forgetting where you are
- Difficulty understanding how you got somewhere
- Confusing past and present
Trouble concentrating or following conversations
- Difficulty focusing on tasks
- Losing the thread of discussions
- Trouble reading or following TV shows
- Mental fatigue during complex activities
Personality or mood changes
- Increased irritability or anger
- Withdrawal from social activities
- Apathy or loss of interest
- Paranoia or suspicion
- Uncharacteristic behavior
Slowed thinking or difficulty making decisions
- Taking much longer to process information
- Trouble planning or organizing
- Difficulty with problem-solving
- Indecisiveness
What to do if you notice dementia-like symptoms
If you or a loved one is experiencing cognitive changes, here’s your action plan, specifically designed for Denver-area families:
Step 1: Don’t panic but don’t ignore it
First, acknowledge that noticing these symptoms is difficult and frightening. It’s natural to feel scared, but remember: early evaluation opens doors to treatment options, whether the cause is reversible or requires management.
Denial helps no one. While some memory changes are normal with aging (like occasionally forgetting names or where you put your keys), consistent patterns of cognitive decline deserve attention.
Step 2: Make a doctor’s appointment
Start with your primary care physician or a geriatrician (a doctor specializing in older adults). Don’t wait for an annual physical – schedule an appointment specifically to discuss cognitive concerns.
Denver-area resources:
- Your current primary care provider
- Denver Health Geriatrics Clinic
- University of Colorado Geriatric Medicine
- Private geriatric practices throughout metro Denver
Many families find geriatricians particularly helpful because they’re specifically trained in age-related conditions and knowledgeable about the many conditions that mimic dementia.

Step 3: Ask direct questions
Don’t be afraid to advocate for comprehensive evaluation. Questions to ask your doctor:
- “Could something else be causing these symptoms besides Alzheimer’s?”
- “Can we check for reversible conditions that mimic dementia?”
- “What tests do you recommend to identify the cause?”
- “Should we review my medications to see if any could be contributing?”
- “Would a referral to a specialist be appropriate?”
- “What’s our timeline for evaluation and diagnosis?”
Step 4: Follow through on testing and referrals
Complete recommended blood work, imaging, and specialist appointments. The inconvenience of testing is worth the potential to identify treatable causes.
Step 5: Consider support resources
While pursuing medical evaluation, connect with local support:
Denver-area resources:
- Alzheimer’s Association, Colorado Chapter
- Area Agency on Aging
- Adult day programs like Sunrise Adult Daycare
- Senior centers throughout Denver
Even if the diagnosis ultimately is Alzheimer’s or another form of dementia, you don’t have to face it alone. Denver has a robust network of support services for seniors and families.
Conclusion
Understanding that many conditions can mimic Alzheimer’s disease is empowering. Not every case of memory loss is Alzheimer’s – some have treatable or reversible causes. The key is getting a thorough medical evaluation that systematically checks for these possibilities.
If you or a loved one experiences cognitive changes:
- Don’t panic, but don’t ignore symptoms
- Schedule a comprehensive medical evaluation
- Ask your doctor to check for reversible causes
- Bring a complete medication list and a family member to appointments
- Advocate for thorough testing if needed
Early evaluation provides the best opportunity for identifying treatable conditions and getting appropriate care, whether that means reversing symptoms or managing a progressive condition with proper support.
Frequency asked questions (FAQs)
Which condition mimics the symptoms of Alzheimer’s disease most often?
Depression and medication side effects are among the most common conditions mistaken for Alzheimer’s. Depression in older adults often causes memory problems and slowed thinking, while many medications can cause confusion and cognitive impairment. Both are treatable.
Which of the following conditions can mimic symptoms of dementia?
Multiple conditions can mimic dementia: urinary tract infections (UTIs), thyroid disorders, vitamin B12 deficiency, depression, sleep apnea, delirium, medication side effects, and normal pressure hydrocephalus. Many of these are treatable or reversible once identified.
Can dementia be misdiagnosed?
Yes. Misdiagnosis can occur when reversible causes aren’t ruled out, comprehensive testing isn’t done, or underlying conditions like depression or medication effects are overlooked. This is why thorough evaluation by specialists is important.
Are there diseases like Alzheimer’s that are reversible?
While Alzheimer’s itself isn’t reversible, many conditions causing similar symptoms are treatable: depression, medication effects, B12 deficiency, thyroid disorders, sleep apnea, infections causing delirium, and some cases of normal pressure hydrocephalus.
What should I ask my doctor if I’m worried about memory problems?
Ask: “Could something other than Alzheimer’s be causing these symptoms?” Request testing for reversible causes like thyroid problems, B12 deficiency, and medication effects. Ask about the evaluation process and whether you should see a specialist. Request a complete medication review.
How long does it take for cognitive symptoms to improve after treating reversible causes?
This varies by condition. Medication-related problems may improve within days to weeks. Delirium often resolves quickly once treated. Thyroid and B12 issues typically take weeks to months. Sleep apnea treatment may show benefits within weeks. Be patient—the brain needs time to recover.




